I want to talk about the recent WHO report on what we have accomplished, what are the current eye concerns / predictions, and the way forward. This report might have been “overlooked” by some of us due to this ongoing surging COVID pandemic and our ( USA ) national elections. Time will tell the adverse affects of this out of control pandemic regarding the prevention / reduction of blindness in the developing world. If the health care infrastructure / support systems are stretched thin in some industrialized countries think of the possible ophthalmic situation / concerns in some low-income countries. Unfortunately eye care in many places have taken a “back – burner” to more pressing Covid-19 issues.
There certainly has been ophthalmic advances in many countries / regions. When we ( my family ) initially moved to Tanzania in the early 1980’s there were few local ( national ) ophthalmologists / ophthalmic surgeons in many sub-Saharan countries. At that time, the ophthalmic infrastructure was not good, at best. Tremendous advances have been made in sub-Saharan Africa, India, Southeast Asia, etc. Many people esp. in the developing world / and many organizations ( WHO / IAPB ) can take some of that credit. However, remember what President Harry Truman said — it’s amazing what you can accomplish as long as you are not concerned who gets the credit. I have tried to remember that over the years.
Years ago,, some eye supplies needed for cataract surgery, etc. were not always readily available. Many ophthalmic supplies/ equipment ( IOL’s, viscoelastics, blades, etc. ) are now being produced / marketed in middle-income countries.
One of the initial IAPB / Vision 2020 The Right To Sight goals were infrastructure / H.R. development. Hard to establish a real sustainable on-going ophthalmic program if there are no ophthalmic nurses / techs trained up / available. Anyway, we certainly have come a long way with many of the WHO / IAPB objectives implemented with Vision 2020, etc. There are some eye physicians / ophthalmic persons in N. America, Europe, and elsewhere who have donated their life work to preventing / reducing / treating blindness in the developing world. We don’t have to re-invent the wheel. In the 1980’s, I can remember a well attended symposium in Tanzania when there was a hotly debated discussion as to whether to supply / insert IOL’s in our east African eye patients. I am not making that up.

However, our work is certainly not done. What continues to be promoted is an integrated people-center eye care ( IPEC ). Years ago, when I lived in sub-Saharan Africa I had a talk on primary health care / primary eye care. This is still being promoted in this report ( 35 years later ). However the two concepts do fit together. If you promote vaccinations then kids don’t contract measles ( ? die ) and hopefully do not end up with blindness secondary to xerophthalmia / keratomalacia. Measles sometimes results in the vulnerable small children ( near starvation ) developing keratomalacia ( ? bilateral ). “ The straw that broke the camel’s back”. In the developing world, vulnerable small kids with acute measles should receive high dose prophylactic Vitamin A to reduce the risk of corneal ulceration. Usually if the starved child shows up with bilateral keratomalacia, then it’s too late. No matter any horrific intervention by the pediatrician it’s too late, the child dies. Night blindness is often present in young children with marked vitamin A deficiency. As mentioned, eye. care must be a part of any universal health care if we are to get to a higher level.
If you push prolong breast feeding ( loaded in Vitamin A ) and routine weighing ( monitoring ) of the infants, then less blindness / deaths from xerophthalmia ( a variant of starvation ) , still one of the leading world causes of childhood blindness. If you give rural villages a continuous reliable source of safe drinking water and with face washing ( S.A.F.E. ) the prevalence of trachoma crashes. There are many correlations between primary health care and primary eye care. When we lived in Malawi, I had a child survival / prevention of blindness project ( USAID ) so I got to do a lot of public health work / activities / symposiums. Good fun. Public health medicine/ intervention is under-rated. In the USA, our ongoing defunding of WHO, CDC, NIH, public health departments / agents at both international, national and state levels has not strengthen our ability to control / contain this surging virus ( Covid-19 ) nor future pandemics. In the future, perhaps with increased funding there might be better initial responses / containment. Currently in the USA, more people have died in the last year ( Jan 2020 – Jan 2021 ) due to this coronavirus than died in WW 2.
Chapter 1. Lists the common eye conditions that do not typically cause vision impairment. The one observation that could be a teachable point is that conjunctivitis ( bacterial / viral/ etc. ) does not cause pain. If the patient was “up all night” with eye pain then the diagnosis is probably not conjunctivitis and the patient might not need an antibiotic / steroid ointment. Perhaps the diagnosis is a foreign body ( flip the lid ), iritis , vascular headache, or rarely acute “glaucoma.” I think that concept concerning eye pain should be taught / emphasized as iritis is often missed, everywhere.
In this report, there was a lot of energy / writing about providing glasses to everyone hopefully to wipe out much low vision. I’m sure that is a worthy cause and certainly the myopic epidemic in Asia and elsewhere is of major concern. However I would like to point out that many people ( patients ) will not wear glasses no matter what. You can show the patient that he /she will see better with the glasses, you can let them walk around with the glasses on, you can give them the glasses ( free ) or sell them at a small price, but the next time you see the patient, he / she is just not wearing the glasses. Right? That was true of many of my patients in Haiti, among the Maasai in East Africa, the Mayan in Central America, etc. I am not knocking it but often the culture / environment/ patient needs are such, they just aren’t wearing your distance glasses. That’s fine but don’t fool yourself on wiping out low vision by giving glasses to everyone. Good luck with that. The PRESENTING distance visual acuity is often more telling than the “ best correction.” As I have mentioned readers are sometimes well received / useful.
In Chapter 1 under risk factors for, and causes of, eye conditions the report mentions many eye conditions are multifactorial in origin. Ageing is a primary risk factor for many eye conditions, so what else is new? People in rural areas are at higher risk of distance vision impairment and blindness than their urban counterparts. Of course, in almost every setting of great poverty, health and healthcare is dreadful. Often the tremendous eye needs are in the rural areas but most of the health workers want to live in the capital or second city as I have written about previously. The spouse wants to live in the big city so she / he can get a job, so junior can go to a good secondary school preparing for university and the family can have a social life. Fair enough. In many emerging countries the visual needs are greatest in rural areas but many eye doctors want a practice treating the middle class / upper middle class in the capital.
One issue that I would like to mention again is please don’t refer blind, hopeless patients when the likelihood of any visual help anywhere is quite poor. You are sending the patient off to the capital or to another country and the prognosis is poor. The family may have to take out a loan or the grandkids have to stop school ( tuition / school uniform fees, etc. ). Perhaps not the best use of limited funds from that family unit.
If you really want to reduce blindness in low-income countries, then reduce poverty. If you are not looking or don’t know what it looks like, then it’s real easy to miss poverty. That’s true everywhere. If you really want good things to happen in a rural community then guarantee an on-going safe source of drinking water. And if we really want to “get down on it”, then ensure 6 years of formal education to all the girls throughout the country. Good things happen with that intervention.
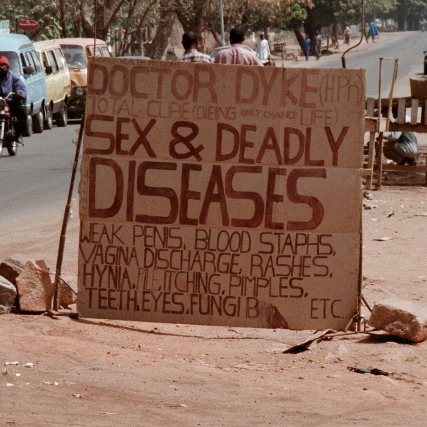
I would like to close now and continue Part 2 of this World Report On Vision on my next blog. The attached photos are of my early work in east Africa. As you can see, some friendly eye competition from Dr. Dyke who appears to have rather extensive medical skills.