This is my guide to the treatment of severe corneal fungal ulcers in low-income and middle-income countries. As we all know, fungal ulcers are more common in the tropics. In the States there are around 1,500 cases yearly —more commonly in warmer humid climates ( southern Florida ).
Fortunately bilateral corneal fungal ulcers are not common but can be a cause for unilateral marked permanent vision loss in our patients. Often by the time the patient presents to the ophthalmologist ( eye MD ) he has already used several topical medicines often with steroids ( chloramphenicol / dexamethasone, etc. ). Often the problem has already been smoldering for 3-4 weeks or more. Sometimes there may not be a history of a minor trauma to the eye ( cornea ) — getting an abrasion with a sugar cane leaf , twig , etc. Sometimes you do get a history of minor trauma with vegetation matter to the eye ( cornea ) — but not always.
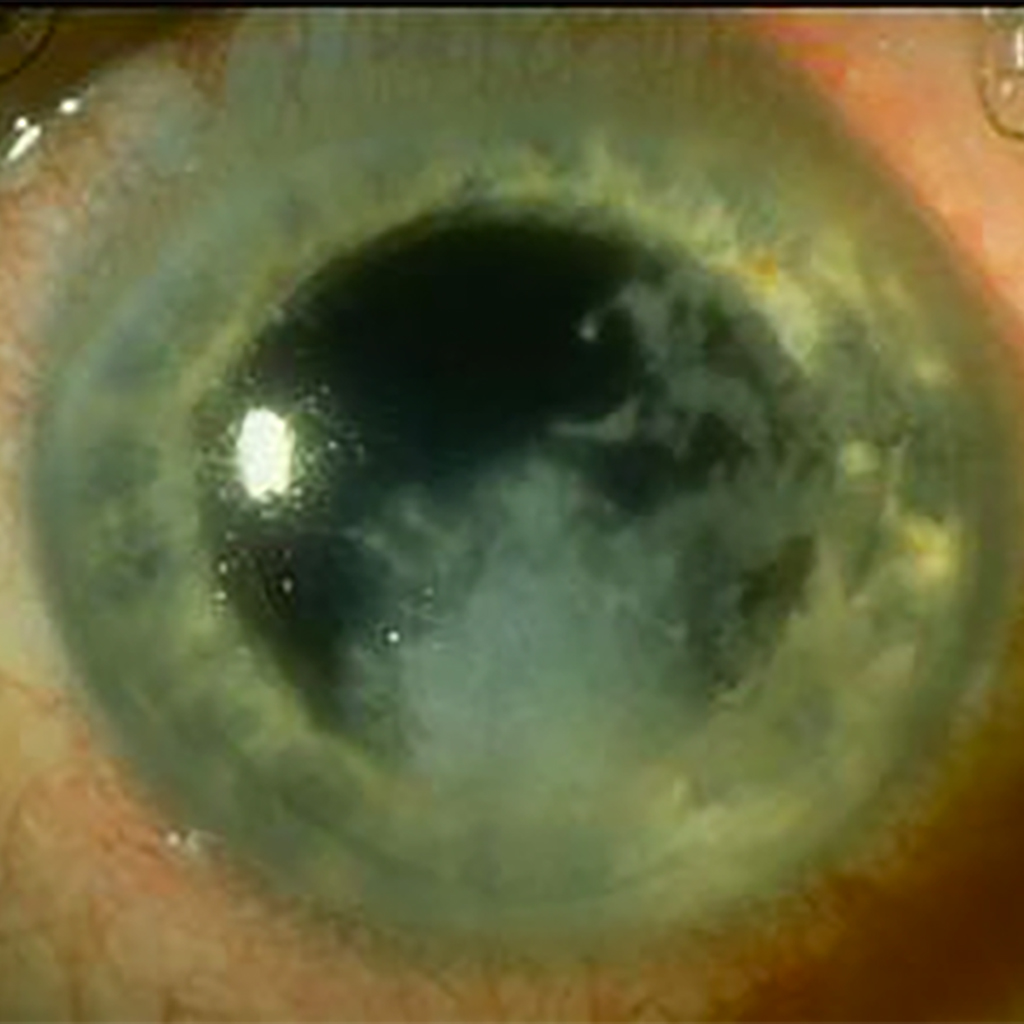
Often the fungal corneal ulcer ( abcess ) is so dense / large you can not even visualize the pupil or iris. Sometimes the deep corneal stromal opacity ( gray-white ) is such you can not determine if there is a hypopyon let alone an endothelium plaque / KP’s or satellite lesions / feathery edges. If the sclera is already involved the prognosis is even worst. This initial active severe / deep corneal presentation is unheard of in North America but certainly not in the developing world. If you look carefully, you might appreciate a descemetocele with a positive fluorescein leakage ( Slidell ) where the cornea might perforate. As many of you know, this is unfortunately not an uncommon initial presentation in the tropics. The problem with fungal ulcers ( filamentous ( Fusarium ) or yeast ( Candida ) is they readily penetrate Descemets membrane unlike most bacteria ulcers where Descemets can act as a barrier to invasion of the anterior chamber.
So I want now to show you what treatments I have used over the last 20 years while living and working in sub-Saharan Africa and elsewhere. Any treatment for this presentation will be long / drawn out. The patient will probably be out of work for six or more weeks and most decidedly have a permanent loss of vision. The patient will need to be on treatment for 12 weeks or longer. You need to have a serious discussion with the patient and his spouse. Almost always these corneal disasters are in males.
Almost all drops that we currently used for fungal ulcers are irritating. You can start off with Natamycin 5% suspension ( shake well ) or amphotericin B ( 0.15-0.30 % ) drops 10 times daily but the patient quickly is using the drops say 4 times daily ( or less ) as the drops burn, sting, and are uncomfortable. That has been my experience when trying to convince these patients to use the drops frequently. Often Natamycin 5% and / or amphotericin B drops ( 0.15% -0.30% ) are not even available in the eye clinic.
What I have done the last several years, after obtaining a history and examining the eyes, is to put a numbing drop in the eye ( pontocaine or tetracaine ), then any antibiotic drop you have, then a dilating drop ( ? atropine ). Then I apply povidone iodine drops ( Betadine ) 5% or 10 % directly to the eye several times.. You should have povidone iodine readily available in the O.R. Then gently mechanically debride / scrap any necrotic superficial corneal material from the ulcer bed. Important. Be sure to remove intact epithelium / necrotic material.
Next I really wet a Q-tip with the providone-iodine solution and gently rub / massage the corneal ulcer. After about three minutes I get another wet / dripping Q-tip and repeat the process of rubbing the cornea with the really wet Q-tip. Applyong Betadine 10% or 5 % every 5 minutes for one hour ( 12 times ) is highly recommended. Numb the eye if necessary.
Povidone iodine is by far the closest thing we have to a universal antiseptic agent. It kills bacteria, virus, fungus, amoeba, protozoa, cysts, trophozoites, etc. Almost nothing is resistant to Betadine.. So really wet a Q-tip / cotton bud ( dripping wet ) and gently rub / massage the corneal with this Q-tip saturated with povidone iodine.
I prepare a 2 1/2% solution of povidone iodine ( 3 ml of povidone mixed with 3 ml of sterile saline or BSS. OK, so now you have 6 ml of a 5% solution of Betadine. OK then add another 6 ml ( BSS ) to that solution and you then have 12 ml total of a 2 ½ % solution of povidone iodine which can be given to the patient to take home I would suggest 10 times daily to start off. Stop any steroid drop / ointment. I have the patient also use a topical antibiotic four times daily. If you have natamycin, amphotericin B or voriconizole, great — use that also.
You can put the 2 ½ % povidine drops in every 5 minutes for the first one hour. Get your staff to do this. Get a loading dose in the eye immediately.
I also start the patient on ketoconzole tablets 400 mg now ( stat ) and then 200 mg twice daily for one month. Have the patient take with Coke or Pepsi as an acid gastric medium greatly improves absorption. Most hospital formulary will have ketoconazole available. If not available then use doxycycline hyclate 100 mg twice daily with food but do not take with milk. The nice think about doxycycline it does also have an anti-inflammation properties and is probably underutilized in ophthalmology. If the hospital has other anti-fungal agents, then consider oral itraconnazole, oral voriconazole
I have not mentioned culturing the corneal ulcer as this is usually not available / possible in low-income countries but a gram stain or Giesma or PAS or KOH might be available /possible and help confirm the diagnosis of fungus .
You might want to consider doing a Gunderson flap on these patients. There are several procedural variations on the Gunderson flap ( You-Tube ) but what is important is just bring down conjuctivae not Teton’s. The flap needs to be quite thin otherwise will retract. Blow up conjunctivae with small amount of Xylocaine 1% with epinephrine initially. The Gunderson flap should be done early on rather than after 4 weeks of intense treatment with no improvement. This is a long treatment process often with little clinical improvement for many weeks.
Anyway, I hope some of this might prove useful. I would welcome other eye care provider’s comments / suggestions.
Peace, Baxter