The case against most corneal transplants in low-income countries.
The problem with corneal transplants in the developing world is that sometimes they are not needed, might result in more eye problems, and often no follow-up care.
It is fairly easy to obtain corneal tissue and bring in a capable ophthalmic surgeon to do the corneal surgery. That’s the easy part. Post-op everyone is congratulating themselves on a clear transplant. But the problem is there often is no post-op care. The patient is often not able to travel for any post-op care, no matter what you think you have set up.
Usually, the only drops the post-op patient will ever have is what you give them on discharge. They probably will not be able to obtain anymore, much less once daily for life as many corneal surgeons recommend post-penetrating keratoplasty. The patient may well not be able to purchase the drops, and the nearest pharmacy could be hours away on foot. If there is any problem ( broken suture, rejection, iritis, ocular hypertension, dehiscence, ulcer, etc, ), it is quite unlikely the patient will quickly see an ophthalmologist, and, if so only after a month or so when the prognosis is now quite poor. And so with any problem, it is possible the graft could fail. Even if the initial post-op concern ( ? broken suture ) was minor.
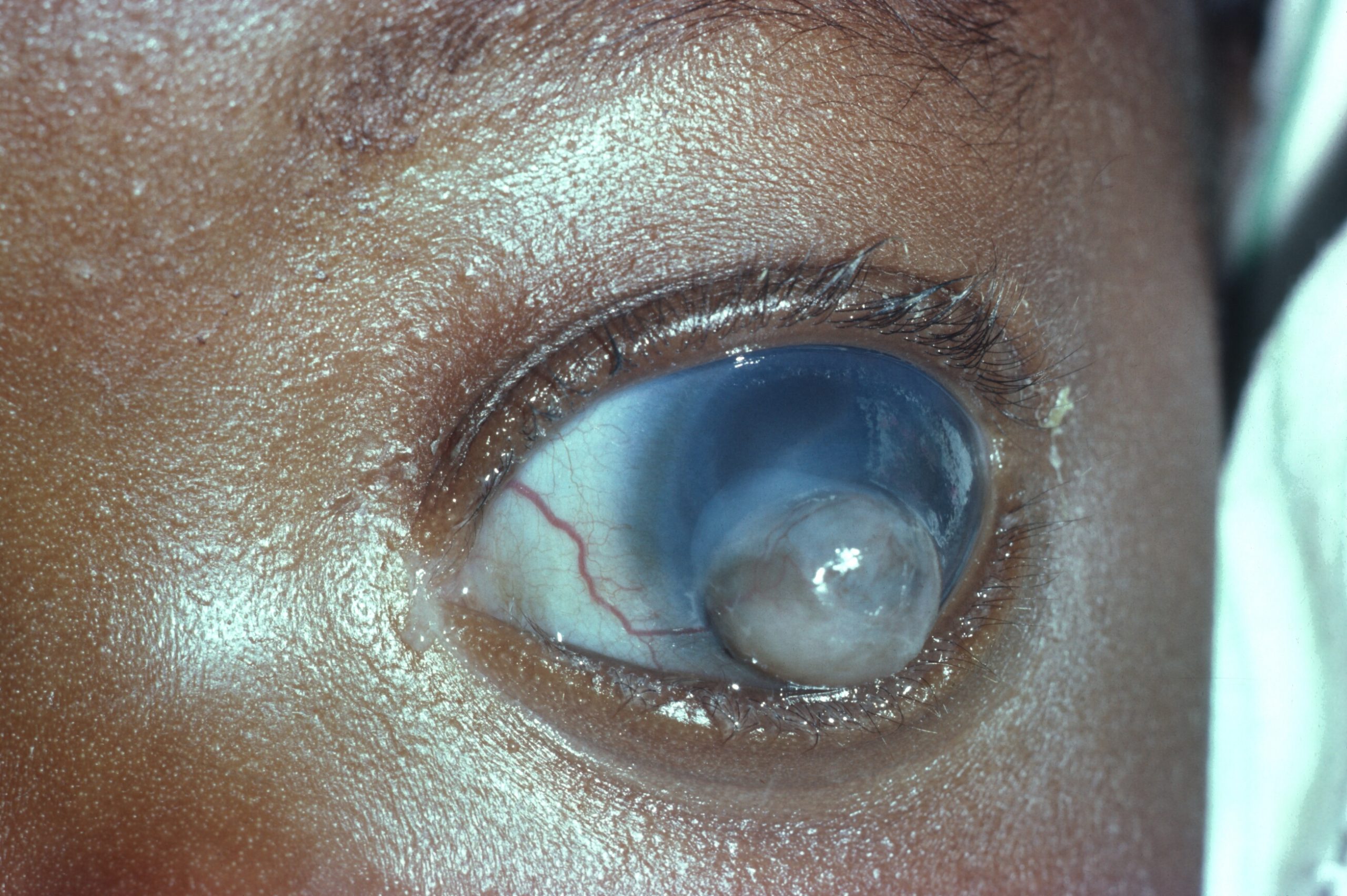
I would suggest if the patient pre-op has 20 / 70 or better in the other ( good ) eye, then don’t do a corneal transplant. If you take an eye ( cornea ) that has an old scar, do a transplant, then a graft rejection, and later bullous keratopathy ( pain, tearing, redness ), then you have not made the patient better, but worst. I have seen this and have written about this previously.
Years ago, when I was the only ophthalmologist full-time in southern Malawi ( 4 million population ) ) a young girl showed up ( with her mother ) with bullous keratopathy from having had a keratoplasty done at an airport in Kenya. I hospitalized her as she had pain, redness, tearing, photophobia, etc. Her well-meaning ophthalmic surgeons had not made her better but worst. Certainly less likely now to snag a husband. The vision in the other ( good ) eye without any correction was 20/20. The mother stated she had previously had an old quiet corneal scar. Terrible. Using North American criteria for penetrating keratoplasty consideration is often not appropriate for the developing world. Many visiting ophthalmic surgeons ( volunteers ) never understand that fully. It took me initially about 6 months of living and working in Tanzania to realize a lot of my western medicine training ( beliefs ) were simply not appropriate for the developing world.
What would really be of interest if you went back 6-12 months after the initial keratoplasties, and, on the patients, you can run down, and record their presenting visions, not their best correction acuity but how they showed up. Record the presenting vision with both eyes open and then each eye separately. Many post-op keratoplasty patients, often have 2 – 3 diopters of cylinder even with a clear graft, so without any correction, what’s the post-op presenting vision?
Don’t get me wrong there are many patients needing a penetrating keratoplasty, but not if the other eye already sees well. Let me give you an example. If you have a patient with bilateral poor vision ( corneal scars ), then a keratoplasty may be indicated. Or perhaps an only eye if the pre-op vision is quite poor. Maybe. Try not to make the patient worst, you know first, do no harm. An Argon laser can often be used to re-make the anterior chamber ( pupilloplasty, etc. ) and improve the vision.
Of course, many developing world patients have poor vision due to bullous keratopathy post-cataract surgery, so endothelial keratoplasty may well be indicated. Difficult to have ophthalmologists show up for endothelial keratoplasty with proper instruments. Unfortunately one of the leading causes of poor vision in the developing world is poor vision post-cataract surgery.
Wealthy patients who already have family in the States or elsewhere in the industrialized world might do better traveling to the States / western Europe where their family members already live. Better post-op options/care.
Anyway, these are my thoughts about penetrating keratoplasty surgery in low-income countries. Some of you may disagree with my opinions.