As far as eye care services there was mention of availability, accessibility, affordability, and acceptability. Persistent inequalities remain between different subgroups of any population in accessing eye care services. In general, those not able to access eye care services as needed include people living in rural areas, those with low incomes, women, older people, people with disabilities, ethnic minorities, and refugees. Many of these issues are sometimes not a concern in the developed world so the depth of these ocular / logistical problems are not fully grasped. Inadequate access to eye care is a major cause of the unequal distribution of eye care. The closer you can bring your eye care to someone’s village, the more likely you are to help that patient, whatever your intervention ( eye surgery, glasses, medication, etc. ). Years ago in Tanzania, when we looked at where our surgical eye patients were coming from, a huge percentage lived less than 30 km from our eye hospital. In other words, we were not reaching most of our rural blind. As we all know, 90% of the world’s blindness are in the developing world.
Poor vision post-cataract surgery is unfortunately not uncommon. As I have mentioned previously, part of this problem is poor pre-op cataract evaluation which can result in disappointment / poor vision post-op. All white cataracts should not have cataract surgery. If you do that, you will most assuredly have some disappointed patients / poor vision post-op. Not a good way to encourage other patients from that village to come for cataract surgery.
Chapter 3 Addressing eye conditions and vision impairment, discusses strategies to address eye care needs — health-promoting, prevention, treatment, etc. As we know, cataract surgery is highly cost-effective. If at all possible the patient should not require numerous pre-op visits to the eye clinic before their cataract surgery. Cost and logistics of travel are major barriers to accessing eye care / surgery esp. for women. The more the pre-op eye patient has to come back / come back, then the less likely that patient will ever have their cataract operation -! come back for blood work, come back for an EKG, come back to see the nurse anesthetist pre-op, come back for the A-scan, etc. Madness.

Trauma is the most common cause of unilateral cataract. If small kids are left unsupervised, then the 5-year-old can hit the three years in the eye with a stick. When that happens that eye usually ends up with poor vision / phthisis. Unfortunately not an uncommon scenario. I do not think I have ever seen any limbal corneoscleral laceration ( ciliary body involvement ) that has recovered any useful vision. These eyes slowly head toward phthisis with a quite low IOP. Right?
When possible, with any visiting cataract surgical safari the outside visiting team should include the local ophthalmologist in the plans / activity so that the local community can see / appreciate that the local ophthalmologist / ophthalmic surgeon is part of the surgical team. It would be good if the in-country ophthalmologist gets to operate. Who knows, it could / should be a learning experience for everyone esp. the visiting surgeons if they do not routinely perform MSICS. With your visiting eye team, you don’t want to undermine the local ophthalmic infrastructure / personnel. You can certainly do that without even realizing that is what has happened.
You want, if possible, to promote the local ophthalmic surgeon as the local eye leader. I have seen / worked in situations where the local ophthalmologist is “ in charge” and often that can be a good model but obviously, that requires a dedicated local ophthalmologist. I have an ophthalmic friend ( now deceased ) who actually paid the local ophthalmologist to be part of his surgical team. Usually, it is a learning experience for everyone and this relationship may ensure reliable follow-up care as needed. Finding / making a lasting relationship / friendship with the local ophthalmic community could enhance everyone’s efforts / impact.
Of interest to me under common conditions amongst adults — Glaucoma treatment: General population screening for glaucoma is not currently considered to be cost-effective in most settings. A couple of times overseas, I have had to remind eye health workers that you really can not screen for glaucoma by just checking IOP. 50 – 50 chance of getting it right — or wrong. I think with eye screening, if you find patients with IOP over 23 mm then these patient should be told they might have glaucoma and when possible referred for further evaluation. Of course a good history might be helpful ( “any one in your family go blind” ? ). Even so, you can miss normal tension glaucoma patients and with a pronounced diurnal variation, as is often common with glaucoma, you may well miss the patient with ocular hypertension / glaucoma. I have repeatedly told eye health workers that checking the IOP a lot and recording the findings are often helpful and quite useful in diagnosing / treating glaucoma. Early glaucoma can be difficult to diagnosis correctly. With a large cup / disc ratio, then if available a OCT / RNFL test can be useful but remember that test may not always be correct. “ Don’t treat the red “. I certainly have seen many patients on one , two or more eye drops who I felt did not have glaucoma but only a large healthy cup / disc ratio. Glaucoma is probably the second leading cause of blindness worldwide. Glaucoma is such a loser that initially ( early on ) IAPB / Vision 2020 did not include glaucoma as a major issue / treatment concern as no one knew how to address glaucoma.. I have seen persons in their 20’s ( Haiti , sub-Saharan Africa ) that have already “ gone blind “ from glaucoma. Dishearting, the number of persons with glaucoma is four times higher in Asia than Africa.
Many of the references at the end of each chapter are of interest to anyone wanting more insight into where we are now and our peer-reviewed literature
Chapter 4 Successes and remaining challenges in eye care. This was written before the coronavirus pandemic so it will be interesting to see what happens in the post-coronavirus ophthalmic world. Many of our projections / long term plans for eye care international will need to be re-assessed in view of this pandemic and the adverse ocular affects in the developing world. Some of the plans / projected challenges might need to be re-thought. The next IAPB meeting should be of interest as we all try to re-group with the way forward.
Mention was made of the adoption of telehealth solutions. No doubt the pandemic has accelerated our use of tele-medicine. The possible of quickly having a second opinion on a complicated eye patient is obviously readily available with our ubiquitous smart phones and many portals including the AAO / ONE program. There is amazing amount of useful information available free through this portal. As most of us know, the International Centre for Eye Health has a twinning program that is ongoing and has helped to enhance the eye care possibilities / treatment strategies / training in many countries / in many eye departments / clinics. Obviously these exchanges are a two way learning opportunity for everyone. More and more informal tele-health consulting are occurring throughout the world. My tele-health problem that I have had with our ongoing diabetic ( retinal ) screening in rural South Carolina is ensuring the 5% with significant diabetic eye findings actually see an ophthalmologist for definite treatment / assessment. If they never get to see an ophthalmologist / eye surgeon , then the program has not accomplished what was hoped. How do you ensure the 5% at high risk , who may have transportation issues, etc. actually receive definitive retinal treatment for their PDR ?
There was mention that increasing life expectancy and population growth will result in additional visual needs / challenges. Some of the issues discussed in this report has been around for decades, many decades. We have made a lot of progress over the last 40 years and there is more to be done. From an ophthalmic standpoint, certainly the ongoing / adverse affects of this pandemic will need to be addressed in the coming years.
Chapter 5 Advancing universal health coverage through eye care. UHC means that all people have access to the health services they need, when and where they need them, without financial hardships. Well I suppose that is a worthy goal. I hope we will one day achieve that in the USA.
Chapter 6 Integrated people-centered eye care. Made reference that ophthalmology is particularly suited to telemedicine. Some of our human resource challenges include general shortages, maldistribution of workers, attrition, imbalances in skill composition and, at times, inadequate regulation. Reference was also made to losing eye care workers to other health sectors ( career opportunities ). That can be a problem if you invest time and efforts to train up the head eye nurse and she gets transfer to a different department as happened to me in Grenada.
Anyway, this concludes the world report. A lot of progress and many issues to be addressed.
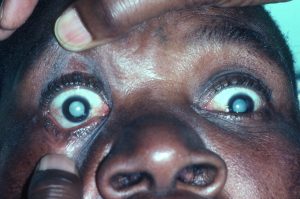
The attached slides are of anterior staphyoma ( thinning and bulging ) secondary to old xeropthalmia / keratomalacia. The other slide show a child with a corneal scar secondary to trauma.
Peace,
Baxter McLendon
]]>There certainly has been ophthalmic advances in many countries / regions. When we ( my family ) initially moved to Tanzania in the early 1980’s there were few local ( national ) ophthalmologists / ophthalmic surgeons in many sub-Saharan countries. At that time, the ophthalmic infrastructure was not good, at best. Tremendous advances have been made in sub-Saharan Africa, India, Southeast Asia, etc. Many people esp. in the developing world / and many organizations ( WHO / IAPB ) can take some of that credit. However, remember what President Harry Truman said — it’s amazing what you can accomplish as long as you are not concerned who gets the credit. I have tried to remember that over the years.
Years ago,, some eye supplies needed for cataract surgery, etc. were not always readily available. Many ophthalmic supplies/ equipment ( IOL’s, viscoelastics, blades, etc. ) are now being produced / marketed in middle-income countries.
One of the initial IAPB / Vision 2020 The Right To Sight goals were infrastructure / H.R. development. Hard to establish a real sustainable on-going ophthalmic program if there are no ophthalmic nurses / techs trained up / available. Anyway, we certainly have come a long way with many of the WHO / IAPB objectives implemented with Vision 2020, etc. There are some eye physicians / ophthalmic persons in N. America, Europe, and elsewhere who have donated their life work to preventing / reducing / treating blindness in the developing world. We don’t have to re-invent the wheel. In the 1980’s, I can remember a well attended symposium in Tanzania when there was a hotly debated discussion as to whether to supply / insert IOL’s in our east African eye patients. I am not making that up.

However, our work is certainly not done. What continues to be promoted is an integrated people-center eye care ( IPEC ). Years ago, when I lived in sub-Saharan Africa I had a talk on primary health care / primary eye care. This is still being promoted in this report ( 35 years later ). However the two concepts do fit together. If you promote vaccinations then kids don’t contract measles ( ? die ) and hopefully do not end up with blindness secondary to xerophthalmia / keratomalacia. Measles sometimes results in the vulnerable small children ( near starvation ) developing keratomalacia ( ? bilateral ). “ The straw that broke the camel’s back”. In the developing world, vulnerable small kids with acute measles should receive high dose prophylactic Vitamin A to reduce the risk of corneal ulceration. Usually if the starved child shows up with bilateral keratomalacia, then it’s too late. No matter any horrific intervention by the pediatrician it’s too late, the child dies. Night blindness is often present in young children with marked vitamin A deficiency. As mentioned, eye. care must be a part of any universal health care if we are to get to a higher level.
If you push prolong breast feeding ( loaded in Vitamin A ) and routine weighing ( monitoring ) of the infants, then less blindness / deaths from xerophthalmia ( a variant of starvation ) , still one of the leading world causes of childhood blindness. If you give rural villages a continuous reliable source of safe drinking water and with face washing ( S.A.F.E. ) the prevalence of trachoma crashes. There are many correlations between primary health care and primary eye care. When we lived in Malawi, I had a child survival / prevention of blindness project ( USAID ) so I got to do a lot of public health work / activities / symposiums. Good fun. Public health medicine/ intervention is under-rated. In the USA, our ongoing defunding of WHO, CDC, NIH, public health departments / agents at both international, national and state levels has not strengthen our ability to control / contain this surging virus ( Covid-19 ) nor future pandemics. In the future, perhaps with increased funding there might be better initial responses / containment. Currently in the USA, more people have died in the last year ( Jan 2020 – Jan 2021 ) due to this coronavirus than died in WW 2.
Chapter 1. Lists the common eye conditions that do not typically cause vision impairment. The one observation that could be a teachable point is that conjunctivitis ( bacterial / viral/ etc. ) does not cause pain. If the patient was “up all night” with eye pain then the diagnosis is probably not conjunctivitis and the patient might not need an antibiotic / steroid ointment. Perhaps the diagnosis is a foreign body ( flip the lid ), iritis , vascular headache, or rarely acute “glaucoma.” I think that concept concerning eye pain should be taught / emphasized as iritis is often missed, everywhere.
In this report, there was a lot of energy / writing about providing glasses to everyone hopefully to wipe out much low vision. I’m sure that is a worthy cause and certainly the myopic epidemic in Asia and elsewhere is of major concern. However I would like to point out that many people ( patients ) will not wear glasses no matter what. You can show the patient that he /she will see better with the glasses, you can let them walk around with the glasses on, you can give them the glasses ( free ) or sell them at a small price, but the next time you see the patient, he / she is just not wearing the glasses. Right? That was true of many of my patients in Haiti, among the Maasai in East Africa, the Mayan in Central America, etc. I am not knocking it but often the culture / environment/ patient needs are such, they just aren’t wearing your distance glasses. That’s fine but don’t fool yourself on wiping out low vision by giving glasses to everyone. Good luck with that. The PRESENTING distance visual acuity is often more telling than the “ best correction.” As I have mentioned readers are sometimes well received / useful.
In Chapter 1 under risk factors for, and causes of, eye conditions the report mentions many eye conditions are multifactorial in origin. Ageing is a primary risk factor for many eye conditions, so what else is new? People in rural areas are at higher risk of distance vision impairment and blindness than their urban counterparts. Of course, in almost every setting of great poverty, health and healthcare is dreadful. Often the tremendous eye needs are in the rural areas but most of the health workers want to live in the capital or second city as I have written about previously. The spouse wants to live in the big city so she / he can get a job, so junior can go to a good secondary school preparing for university and the family can have a social life. Fair enough. In many emerging countries the visual needs are greatest in rural areas but many eye doctors want a practice treating the middle class / upper middle class in the capital.
One issue that I would like to mention again is please don’t refer blind, hopeless patients when the likelihood of any visual help anywhere is quite poor. You are sending the patient off to the capital or to another country and the prognosis is poor. The family may have to take out a loan or the grandkids have to stop school ( tuition / school uniform fees, etc. ). Perhaps not the best use of limited funds from that family unit.
If you really want to reduce blindness in low-income countries, then reduce poverty. If you are not looking or don’t know what it looks like, then it’s real easy to miss poverty. That’s true everywhere. If you really want good things to happen in a rural community then guarantee an on-going safe source of drinking water. And if we really want to “get down on it”, then ensure 6 years of formal education to all the girls throughout the country. Good things happen with that intervention.
I would like to close now and continue Part 2 of this World Report On Vision on my next blog. The attached photos are of my early work in east Africa. As you can see, some friendly eye competition from Dr. Dyke who appears to have rather extensive medical skills.
]]>The patient had a dense white cataract on the right with superior posterior synechiae between 11:00 to 1:00 PM. On the left the patient had an inferiorly subluxated pc IOL, a macular scar, and old retinal laser marks. There was no view of the right posterior pole due to the mature cataract. The eyes were quiet (no A.C. cells, etc.) with normal IOP’s OU and corneas.
With the mature right dense cataract, I immediately went into my three-step test mode. #1. Color vision was normal. Sees red ( filter ) color as red. #2. No relative afferent pupillary defect (RAPD). #3. But poor light projection even with a dilated pupil. He could not identify / localize / point to where the light was originating.
I advised patient that we could operate on his right cataract but he could have other problems behind the right dense cataract such as a retinal detachment. Then he sheepishly stated that previously in Ca. he was told he had a retinal detachment OD and yes previously he had had laser treatment / surgery OS.
So my point is, as with this patient, this three-step (90 seconds) test will often rule in or rule out eye pathology behind a dense cataract. Leave the B-scan in the States. All white dense cataracts should not immediately have cataract surgery. If the patient can’t see the color red (pink, orange, even yellow is acceptable), don’t operate. If they have a relative afferent pupillary defect (RAPD / Marcus Gunn pupil), don’t operate. If they have poor light projection with a dilated pupil, don’t operate.
You don’t have to make the diagnosis only the prognosis of improving the vision after cataract surgery. Right?
Incidentally, often with a old R.D. the patient has hypotony which was not the case in this patient.
Peace, Baxter
]]>Lots happening in global ( international / tropical ) ophthalmology at this time. More interest in efforts to reduce / prevent blindness in the developing world. There are now more physicians / eye health care personnel that have become interested in the efforts of IAPB, Vision 2020, twinning programs, and ophthalmic NGO’s everywhere, etc.. Certainly more courses / symposiums at the Academy concerning the way forward in the reduction of world blindness.
There are many people ( ophthalmologists ) who for decades have been “ waging war against blindness” throughout the developing world. A few North American ophthalmologists ( and more Europeans ) have given their life work to the improvement of the ophthalmic situation in the developing world. We do not have to re-invent the wheel — what works overseas, what is appropriate, what is sustainable, what can be done to strengthen ( not weaken ) the local ophthalmic infrastructure, how do we reduce the brain drain, how to prevent repeating previous mistakes, etc.. Ophthalmic human resource growth and infrastructure development have made incredible advances over the last 30 years. Much good work has been accomplished over the last 3 – 4 decades and much needs to still happen in the new decade( s ). There are many local ophthalmologists / eye health providers that are now taking the lead in eye care in their home countries / regions. Good. With all the chaos coming out of Washington, with the increasing concerns about the effects of climate change secondary to man, it is easy to forget/ discount the tremendous efforts / accomplishments that have occurred over the last 30 years regarding eye care in the developing world. Do you think climate change is having a negative impact on our global eye efforts?
If you have a real interest in Global Ophthalmology then I would encourage you to attend the WOC meeting in Cape Town in June 2020, especially the IAPB meeting in Singapore in October 2020, and the Academy annual meetings ( Global Forum / SEE, Seva, IEF, HCP, Orbis receptions, etc. ). 2020 is a special year for our ongoing efforts to reduce blindness. How can we get the best impact for our efforts — the best bang for our limited health ( eye ) care bucks.
With the beginning of a new decade, I would like briefly to mention some deceased ophthalmic ( global ophthalmologists ) greats who I have fortunately known ( met ) and who have over many years helped to move the goal forward — Fred Hollows, Barry Jones, Jim Standerfer, David Apple, John Cheatham, Joe Taylor, Marilyn Scudder, and many others. Many unsung ophthalmologists have worked tirelessly for decades to reduce blindness in low-income/ middle-income countries. Of course there are many still in the fight — still pushing to reduce blindness among the poor in emerging countries. A good example would be Marilyn Miller MD who this year ( 2019 ) received the AAO Laureate Award to a standing ovation, and Larry Schwab MD who next year ( 2020 ) will receive the International Blindness Prevention Award. Congratulations to you both.
It will be interesting to attend the 2020 IAPB meeting and for all of us to help plot a way forward for the new decade. How can we work together to reduce / prevent blindness? As Barry Jones once said, there are enough poor blind patients in the world for all of us to service. Of course, as we all know, if you want to reduce blindness, then just reduce poverty and give all the girls at least six years of formal education. Now that’s an intervention worth pursuing.
I would like to suggest that complicated eye patients in developing world countries not be referred somewhere for further eye care / consultation when there is really no realistic treatment / intervention possible for that patient and his / her disease process. “ Things “ often do not work in low-income countries / cultures as in industrialized countries. Better for the family to spend their money on school tuition / uniforms / food rather than sending grandmother to the capital or out of the country for further medical evaluation ( $$$ ). Most of my patients in Belize, have a “bad experience” trucking off to Mexico or Guatemala for further eye care/ evaluation. Easy to unload the patient / health problem by referring away but what really is best for the patient and that family unit ?
I have written on this previously but would suggest you not carry used / rehab glasses from the States. Most patients in developing world countries simply do not want used glasses even if they might see better. Reading glasses are often well received but usually not other glasses. They eventually get tossed out. Also many patients who could actually see better with glasses simply will not wear them. This is true in many countries / cultures. Unfortunately we will not prevent / cure low vision by giving everyone a pair of glasses

Western medical mentality is often not correct for emerging – world countries. It took me a couple of years of living and working in Tanzania to understand partially that concept. I’m still learning. Let me give you an example before I close. The attached photos show one patient with bilateral dense cataracts. So operate on either eye ( cataract ), correct? But how about the other patient with dense cataracts OU but a subluxated lens OS? The history could be useful. OK, so which eye ( cataract ) do you operate on first? In the States you could certainly make the case for operating on the left eye ( don’t forget the IV mannitol ), see what vision post-op you achieve and do the right ( good eye ) eye at another time. That would be reasonable for most of us in the States. But what if this is the only chance for this patient to gain useful vision? One chance and the patient will never see another eye surgeon. Often tremendous efforts / cost for the family to show up at your eye center / O.R.. One chance. So which eye do you now want to operate on? In the developing world operate on the right eye. You want to operate on winners. Blind before surgery and perhaps blind after surgery is not good for the patient, the family, or the ophthalmic P.R. for that community.
I wish you all a happy / useful 2020. Get involved. Be here now.
Keep The Faith,
Baxter McLendon MD
803-632-1699 Home
803-591-8332 Cell
If you take a patient with poor vision but otherwise an asymptomatic eye, operate, and end up with a permanent bullous keratopathy then you haven’t helped the patient. I have seen that scenario on a number of occasions. Unfortunately, I certainly have been guilty of that myself.
Over the years I have seen many patients in the developing world who have had a penetrating keratoplasty which has resulted in a failed graft, bullous keratopathy, and an eye that is uncomfortable, tearing, inflamed, photophobic, and symptomatic. Often the vision is worst post-op [ blind painful eye ]. There are many exceptions but as a general rule corneal transplant patients do not do well in evedevelopingld situations especially low-income countries.
The problem is not the operation. There are many skilled ophthalmic surgeons who can do a great corneal transplant in a developing world setting. The problem is what happens post-op. The long term post-op care is often lacking or non – existent.
The best candidate for a corneal transplant in the developing world is someone financially well off, living in an urban setting with quick easy access to advanced ophthalmic care. If the patient has limited [ finances ] resources, lives in a rurally isolated area, and does not have quick ready access to ophthalmic care and medicine [ drops ] then the graft is often doomed to fail. I have seen this over and over again in the developing world. If the post-op patient develops a graft rejection, corneal ulcer, uveitis, ocular hypertension, suture breaks, wound dehiscence, etc. bad things can happen, resulting in a failed graft. The post-op corneal transplant patient with a problem usually shows up quite late if at all.
If the patient has good vision in the other eye, I suggest not doing a corneal transplant. I would go real slow in bring a child or adult to the developed world [ USA ] for penetrating keratoplasty. Within the last two weeks in Belize, I have seen a young female patient who was taken to the States several years ago for a corneal transplant in her only eye. According to our rehab folks she apparently had pre-op light perception vision and an asymptomatic eye. She is now NLP with severe pain.
Often what a young person doesn’t like about a unilateral opaque cornea is the cosmetic appearance. These patients may be candidates for corneal tattooing [ Indian ink ] and therefore making the opaque white cornea brown to match the other eye [ iris ].
If you are dealing with the only eye, then sometimes [ rarely ] an autocorneal rotation will move a clear peripheral corneal segment into the visual axis and an opaque [ scar ] central cornea into the periphery. This opportunity doesn’t occur often but can be quite successful [ no rejection ]. You will not end up with 20 / 20 vision but perhaps 20 / 70 without correction.
A surgical option in the only eye scenario is to do an optical iridotomy [ pupilloplasty ]. If you have the iris stuck up to the endothelium [ adherent leucoma ] just make a new or larger pupil. Don’t mess with the adherent leucoma. Let that sleeping dog lie. Use a lot of viscoelastic and long blade van Ness scissors or other anterior segment scissors. Often a little snip is all you need. Don’t get carried away. Don’t cut out anything [ bleeding ]. Often the crystalline lens is clear.
Another option is using an Argon, diode or Nd – Yag laser. First, apply pilocarpine 2% times three. Make a radial laser-cut either nasally or laterally depending on the situation/location of the corneal scar. Cover post-op with brimonidine [ Alphagan ], acetazolamide [ Diamox ], or whatever. Post-op cyclopentolate and steroid drops are useful.
In conclusion, I would be slow to recommend a corneal transplant to a poor patient in the developing world. It’s not the operation itself but the long term post op care that is the problem.
Peace,
Baxter
]]>Over the last 15 years plus of operating on mature cataracts, I have not uncommonly encountered an iris prolapse during the operation. Usually, this is near the beginning of the operation. There certainly can be many causes for this — a beginning choroidal hemorrhage ( rare ), to poor wound construction [ fairly common ], the fluid trapped behind the nucleus or iris, and other causes.
With the MSICS, if you make your entrance into the anterior chamber too peripheral ( prematurely ), then you might have an ongoing iris prolapse throughout the rest of the operation. Wound construction is important with the clear cornea or also corneoscleral tunnel incisions.
Sometimes just changing surgical positions ( starting over ) at a different limbal location is the best course although surgeons are sometimes reluctance to begin again in a different location. You can put in a suture to reduce the size of your wound during I and A which is often when the iris prolapses reoccur.
You can try rotating or rocking the nucleus in case fluid is trapped behind the cataract but in my hands that usually is not helpful. You can reduce the pressure on the globe from the lid speculum but usually, that is not the problem.
However, if I get an iris prolapse, the first thing I do is to do a one snip radial full-thickness iridotomy. Just make a hole in the peripheral iris. You are not removing any iris [ iridectomy ] but rather just making a hole ( iridotomy ). If you look carefully through the slit lamp you will often see a small gush of fluid from the posterior chamber through the newly created iris opening ( hole ). If you get the gush then often the iris will simply fall back and no longer prolapse. This does not always solve the problem but often it will and worth the attempt/effort. It is fairly safe.
Be careful to make the hole in the iris toward the base/periphery of the iris and not near the pupil. You want a full-thickness cut ( opening ). It is quite easy to cut closer to the pupil than you want.
I would encourage you to try this as often the one snip full-thickness iridotomy will solve the problem with the iris prolapse.
Peace,
Baxter
]]>IAPB, 9th General Assembly
Eye Health: Everyone’s Business
September 17-20, 2012 Hyderabad, India
The IAPB is an umbrella coordinating organization of over 120 members which was founded in 1978 by Sir John Wilson for the reduction, prevention of avoidable blindness and visual impairment, especially in the developing world. Under Dr. Mario Tarizzo the World Health Organization’s Programme for the Prevention of Blindness was established in 1978. These two organizations started the global initiative Vision 2020, The Right to Sight in February 1999 to eliminate the main causes of avoidable blindness in order to give all people in the world, particularly the millions of needlessly blind, the right to sight. The strategy of Vision 2020 is built upon a foundation of community participation, with three essential components:
- Cost-effective DISEASE CONTROL interventions
- HUMAN RESOURCE DEVELOPMENT ( training and motivation ).
- INFRASTRUCTURE DEVELOPMENT ( facilities, appropriate technology, consumables, funds ).
Below I would like to share some observations/lessons learned while recently attending the IAPB 9GA meeting in Hyderabad, India. These notes represent the thoughts /opinions/publications of many speakers/organizations. I have borrowed freely from many of the speakers for this summation.
- Non-communicable diseases ( NCD ) are the single biggest cause of deaths worldwide. NCDs include CVD, diabetes, cancer, COPD, tobacco usage, excess alcohol, etc. With tobacco usage, there is an increased incidence of cataracts, glaucoma, and ARMD. In Australia, there has been a media campaign with the message: Smoking Causes Blindness. Check out the website. I have printed one of their posters to display in my eye clinic in Belize.
- More diabetics worldwide will live into old age. Diabetics are 25 times more likely to go blind. Currently, 84% of the world population resides in the developing world. By 2050, 80% of the elderly will live in developing countries. The potential adverse interaction between uncontrolled diabetes, hyperlipidemia, and hypertension need to be publicized widely. International Diabetes Federation < www.idf.org.> is an umbrella organization for many diabetic associations.
- There was a lot of discussion about sustainability eye programs. Various successful models from around the world were presented. Usually a three-tier system: 1. the poor receive free eye care/surgery. 2. the financial middle class receive subsidized services, and the wealthy pay a larger ( full ) amount sometimes with ” special treatment ” but everyone receives high-quality care. The cost for an eye visit ( exam ) is no more that one day’s pay and the cataract surgery cost is no more that one month’s pay (salary).
- Cataract surgery coverage in the developing world is usually worst in rural areas. Most of the ophthalmic care (providers/infrastructure) is concentrated in the larger cities and the overwhelming need/population is usually in rural areas. Who is usually underserved are women and the poor in rural areas? ( What else is new ) ?
- Cataract surgery coverage ( CSC ) is a coverage indicator. Uses the operated persons in the community as the denominator. Measures accessibility and utilization of services at the community level. It requires a population-based survey which is usually expensive.
- If there had been no WHO / IAPB / Vision 2020 interventions then the blindness ( <6/60 or < 10 degree V. field ) prevalence prediction was 76 million by 2020. However, the most recent 2010 WHO figures are 39 million blind ( < 6/ 60 ) , 246 million with low vision ( < 6/ 18 ), for a total of 285 million. The top five causes of blindness worldwide are cataracts, uncorrected refractive errors ( URE ), glaucoma, childhood blindness, and diabetes. Unfortunately, many patients are still blind after cataract surgery. Ongoing success stories are onchocersiasis, trachoma, vitamin A ( xerophthalmia ) deficiency, and cataracts in some places like India.
- The barriers to achieving the goals of Vision 2020 in middle-level ( developing ) countries are mainly political. Need increased commitment of national governments. Now we need serious discussions with national Ministries of Health. Governments must buy-in.
- Cataract surgical rate ( CSR ) represents the number of cataracts operations ( eyes ) per million population per year. A good indicator of output. CSR requires proper record keeping to know where patients reside, etc. Country-level CSR often hides regional inequalities. So what is the ideal CSR? Target CSR should at least equal annual incidence of cataract. Otherwise, the cataract backlog may increase. Different V.A. criteria for cataract diagnosis will require different CSR’s. For many developing countries a CSR between 1500 to 2000 is ideal. Often difficult to determine true CSR as providers ( surgeons ) sometimes reluctant to reveal their CSR.
- Primary health care and primary eye care ( PEC ) go together. So what is PEC? : access to clean drinking water ( decrease trachoma ), increase vaccination ( decrease blindness from measles ), prolonged breastfeeding/infant weighing ( decrease xerophthalmia ), increase CSR ( decrease poverty, increase/prolong schooling for children in that family unit ).
- The International Society of Geographical and Epidemiological Ophthalmology met after the main IAPB meeting with a theme of Vision 2020 – The Countdown Begins. Professor Allen Foster gave Elizabeth Cass Oration 2012: Neglected Tropical Diseases and Vision 2020.
- Non-compliance for glasses is almost 100% in children with small refractive errors ( -1.00 to + 1.00 D ) The higher the refractive error, the more likely the child is to wear glasses. Compliance is less after 6 months compared to one month. Girls are more likely to wear glasses than boys.
More to come. Hope some of this is useful.
Baxter McLendon MD
]]>IAPB, 9th General Assembly
Eye Health: Everyone’s Business
September 17-20, 2012 Hyderabad, India
– Part 2 –
- Barriers to cataract surgery:
- Unaffordable cost ( surgery / IOL , consultations, lab / EKG, transportation, accommodation, etc. ).
- Family concerns ( no one to accompany patient ).
- Logistic issues.
- Fear.
- Ignorance.
- Other diseases prevent cataract surgery.
- The 200,000 worldwide ophthalmologists are not adequate for future needs. Today 6 million cataract operations yearly. The number of persons over age 60 years is growing faster than the # of ophthalmologists. In many countries, 50% or more of the ophthalmologists do not perform cataract surgery.
- More blindness ( percentage ) secondary to corneal opacities/injuries ( unilateral and bilateral ) in the developing world.
- In some ocular surveys, the leading cause of blindness is cataracts and the second leading cause is blindness after cataract surgery. Monitoring surgical outcomes are important and were a major theme of this IAPB meeting. Surgical outcomes are important, just as important as CSR. Unfortunately, bad outcomes ( poor V.A. ) after cataract surgery are not uncommon. Good quality is essential to generate demand. Must not compromise quality. Basic minimum standards often lacking in developing the world. Monitoring and evaluation are important from the get to go.
- The Fred Hollows Foundation ( Australia ) and Price Waterhouse Cooper have demonstrated that the benefits of eliminating avoidable blindness and visual impairment far exceed the investment required. In developing countries, the estimated benefits outweigh the costs by a multiple of 4.1. In addition, there were other benefits such as the substantial gains in quality of life for the patient and their caregivers ( families ). Quality of life improvements includes increased primary education for any children within that family, reduced extreme poverty, increased independence/self-esteem, improved social networks, and increased gender equality.
- The most dangerous animal in subSaharan Africa other than man is not the hippo, the lion, nor the elephant but rather the mosquito ( malaria, yellow fever, Dengue fever, lymphatic filariasis, and some viral encephalitides ).
- The World Bank has been involved in eye care and wants to do more. Cataract surgery has been identified by the World Bank as one of the most highly cost-effective strategies that can be offered in developing countries The transmission ( black fly ) of Onchoceriasis may be eliminated by 2025.
- Human resources are the most expensive part of any health care program.
- Vision 2020: The Right To Sight’s goal to eliminate avoidable blindness by 2020 will not be achieved by acting alone. Need to bridge the gap. One size will not fit all in implementing Vision 2020. Huge opportunity to work more closely with other health care developers/organizations. Pick your partners carefully.
- Do not take/send broken eye equipment to developing world countries. Make sure the equipment is working and ship spare parts of the most likely problems. Non – working equipment is often worthless as there is no one to repair the equipment ( bioengineer, handyman, etc. ), no spare parts, no warranty, no hard currency to purchase broken parts from overseas, etc. Send the manual of any equipment shipped.
- Results from Peru and Belize show that the standardization of knowledge in oxygen therapy for caregivers in the NICU decreased the number of RoP babies and also the RoP infants needing treatment. Currently, the prevalence of blindness from RoP is the highest in middle-income countries
- Many of the various ophthalmic non-government developmental organizations ( NGO’s ) gave update reports of what they were doing worldwide to eliminate avoidable ( neglected ) blindness. Also updates on prevention of blindness efforts in South Asia, subSaharan Africa, and Latin America.
- SAFE strategy for trachoma: Surgery ( tarsal rotation ), Antibiotics (azithromycin ), Face cleanliness/ washing, and Environmental improvement have had a tremendous impact on the reduction of trachoma. Currently 63 million treatments with azithromycin ( Pfizer ). The most active trachoma currently is in Africa. < WWW Trachomaatlas.org> for world map of trachoma. GET 2020: Global Elimination of Trachoma as a blinding disease by 2020.
- Don’t talk about blindness but vision. Talk positive, not negative
I know this might have been a little disjointed but hope some of my notes were useful
Peace,
Baxter McLendon
]]>Vol. 60, No.5 / Sept 2012
Click here for Free Full Text
In conjunction with the 9th General Assembly 2012 of the Int. Agency for the Prevention of Blindness ( IAPB ) Hyderabad September 2012 — Eye Health: Everybody’s Business, the Indian Journal of Ophthalmology ( IJO ) dedicated their Sept. 2012 issue to the prevention of blindness, worldwide. I would like to review this special issue of the IJO which was actually given out at the Hyderabad assembly. As previously, I will draw closely on the observations/ comments of many of the authors. Please note that credit will not always be acknowledged to these international ophthalmic leaders. However, the free full text is available online <http://www.ijo.in/showBackIssue.asp?issn=0301-4738;year=2012;volume=60;issue=5;month=September-October>.
There is currently no greater eye success story than the all- Indian efforts to reduce the prevalence of blindness in India. India’s cataract surgery figures increased dramatically from about half a million in 1980 to more than six million by 2010. This greater than 10-fold increase has handily exceeded the previously dreaded incidence of three million new cataract cases each year. In fact, many eye success stories in disease control/prevention have been achieved throughout the world ( Onchocerciasis, RoP, WHO Global Elimination of Trachoma, etc. ).
S. Natarajan ( editor, IJO ) gave a good overview of milestones in the Indian blindness prevention efforts. He discussed where we are and where we need to travel with our international blindness reduction efforts. Al Sommer with a guest editorial gave a brief succinct history of the IAPB and the way forward. Much has been accomplished, much still needs to happen.
The largest obstacle faced in the fight against blindness in different parts of the world is the lack of access to good quality and to affordable eye care services, especially in isolated rural areas. Urban dwellers are far more likely to receive eye care/ surgery than those in rural areas.
There was an article by Bruce Spivey and other Int. Council of Ophthalmology ( ICO ) players concerning the training of ophthalmic residents in the concepts and the practice of community eye health ( CEH ) which incorporates primary eye care and a public health approach to the main causes of blindness and low vision. The upcoming version of the ophthalmological residency curriculum that was developed by the ICO includes a new specific section on CEH.
Health inequality refers to differences or inequalities in health among social groups that are unnecessary, avoidable, unfair, and intolerable. These inequalities are related to social determinants based on gender, socioeconomic status, ethnicity, race, or having a specific health condition. Inequality, poverty, exploitation, violence, and injustice are causes of illness (blindness) and death of the poor and marginalized.
Eye care inequality exists in a variety of ways around the world. Many sub-Saharan African countries still have only one ophthalmologist per one million persons and the goal is to reach a ratio of 1 per 250,000 persons by the year 2020. There is a common social gradient across global society — the lower the socioeconomic position of an individual, the poorer their health. This is probably also true in industrialized countries. With regard to gender inequality, women have a higher prevalence of visual impairment and blindness which can not be explained based only on age or access to service.
There was an article [ Ravilla ] on advocacy for eye care which can be a useful strategy for all of us in the developed and developing world. Examples given were diabetic retinopathy and pediatric eye care.
An excellent article by Peter Ackland, current president of IAPB, outlined the accomplishments of the global initiatives Vision 2020: The Right to Sight and the focus for the next 8 years of the campaign. Dr. Acland discussed where we have been, where we are, and what needs to happen in the next eight years. We need more programs, better programs, and faster progress toward our goals.
To achieve the goals of Vision 2020 considerable scaling up of current efforts will be required. Two key areas will be:
- Successful advocacy and engagement at the individual country level for enhanced national government commitment to finance their own Vision 2020 plans and
- A new approach to Vision 2020 thinking that integrates eye health into health system development and develops new partnerships with wider health development initiatives. Two separate health programs were mentioned— the Neglected Tropical Disease movement and the Non-Communicable Disease ( NCD ) movement.
Well, I hope my last several blogs on the international effects to reduce blindness have been interesting and also informative. There are a lot of persons and organizations that have contributed to our ongoing success.
Peace,
Baxter
]]>Margaret once told me she had saved many eyes in India by using a Gundersen flap. With a truly bad cornea — marked diffuse abscess ( ? fungal, ? herpes, ? bullous ), a large indolent chronic ulcer, descemetocele, etc., a Gundersen conjunctival flap can often save the eye. Furthermore, if you have a phthisical eye, first doing a Gundersen flap might allow you later to fit an overlying prosthesis. Trygve Gundersen MD first described this new conjunctival flap in 1958.
First do a peribulbar( anesthetic ) injection, then a subconjunctival injection superiorly ( lidocaine 1% or 2% with epinephrine 100,000 – 200,000 ). Blow up the superior bulbar conjunctiva but do not pierce the conjunctiva in the areas to be used for the flap. Next gently remove the entire corneal epithelium either with a # 15 blade or a sterile cotton applicator ( Q tip ) wet with BSS, or a topical antibiotic, or 5% povodine – iodine (Betadine) or diluted rubbing ( isopropyl ) alcohol. Do not disturb limbal stem cell areas. Debride necrotic tissue. Many surgeons utilize an inferior intracorneal traction suture if necessary.
You want to bring down only the bulbar conjunctiva — either excise or leave behind Tenon’s capsule. Undermining, freeing up the conjunctiva takes time if done correctly. Avoid buttonholes. You need a loose large thin mobile superior conjunctival flap. Do not drag down Tenon’s fascia as that will result later in retraction of the flap. You do not want any tension/traction on the flap. If you can not easily get the conjunctival flap down to the inferior limbus then make an inferior peritomy, undermine, and bring up the lower bulbar conjunctiva to cover the inferior 2 – 3 mm of the cornea. You can also do a 360-degree peritomy with relaxing incisions.
I like 10-0 nylon sutures either interrupted, running or both. Some surgeons prefer larger absorbable sutures at both superior and inferior limbal areas. In the end, dilate the pupil and cover with an antibiotic ointment. Leaving a pressure patch on for 48 hours reduces post-op chemosis.
Most experienced corneal specialists that I have questioned, would do a Gundersen flap over a descemetocele. Obviously, you are less likely to appreciate a corneal perforation and / or a flat A.C. with a Gundersen flap covering the cornea. Stored glycerol cornea suitable for a patch graft is sometimes available. The Alabama Eye Bank <[email protected]> has free sterile glycerol corneas available in limited amounts for the developing world ( patch graft only ). Some centers use sclera as the patch graft material.
Gundersen conjunctival flaps are now used infrequently where a therapeutic penetrating keratoplasty is an option. However, I would strongly recommend this procedure. As noted by Dr. Brand you can save many eyes and avoid an evisceration. If the patient still has light perception vision and can still see the color red ( color perception ), they may well be a candidate for a Gundersen flap.
Peace,
Baxter McLendon
]]>